Diabetic Care
Diabetic Care
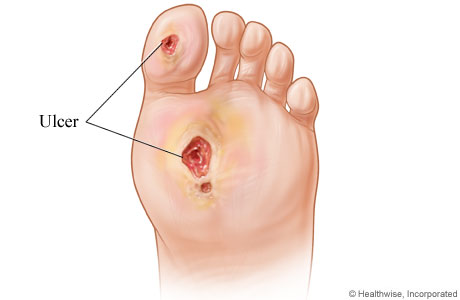
Call to manage your Diabetic care today, or Schedule an appointment. Diabetes is the leading cause of non-traumatic lower extremity amputations in the United States, and approximately 14-24 percent of patients with diabetes who develop a foot ulcer will require an amputation. Foot ulceration precedes 85 percent of diabetes-related amputations. At OCFA we can help you starting TODAY with your Diabetic Foot and Wound Care.
RELATED LINK: Diabetic Shoes with Medicare & PPO
Diabetic Footcare Information with Dr. Daphne Yen of OCfeet.com This is a top podiatry service provider in Orange County, California.
What is a Diabetic Foot Ulcer, What causes ulcers in a diabetic’s foot?
A diabetic foot ulcer is caused by neuropathic (nerve) and vascular (blood vessel) complications of diabetes. Nerve damage due to diabetes causes altered or complete loss of feeling in the foot and/or leg. This is known as peripheral neuropathy.
RELATED PAGE: Diabetic Peripheral Neuropathy

Research shows that a foot ulcer is preventable. Allow us at OCfeet.com to work with you in partnership to manage your Diabetic Foot & Wound Care.
Healing in Diabetic Foot Ulcers: Epifix
EpiFix is a bioactive tissue matrix allograft composed of dehydrated human amnion/chorion membrane (dHACM) that preserves and contains multiple extracellular matrix proteins, growth factors, cytokines, and other specialty proteins.
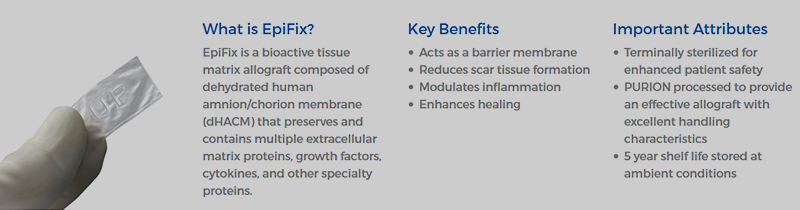
EpiFix is intended for homologous use to reduce scar tissue formation, modulate inflammation, enhance healing, and act as a barrier membrane. EpiFix is processed through the proprietary PURION® process that protects the delicate scaffold during processing, leaving an intact collagen matrix. The result is a durable, bioactive allograft with natural barrier properties which may be stored at ambient conditions for up to 5 years. EpiFix is available in sheet, mesh, and particulate configurations and in a variety of sizes to reduce wastage.
EpiFix is processed from human tissue according to the American Association of Tissue Banks (AATB) standards, and is regulated as a human cell, tissue, or cellular or tissue-based product (HCT/P) under Section 361 of the Public Health Service Act.
Causes:
Anyone who has diabetes can develop a foot ulcer. Native Americans, African Americans, Hispanics, and older men are more likely to develop ulcers. People who use insulin are at higher risk of developing a foot ulcer, as are patients with diabetes-related kidney, eye, and heart disease. Being overweight and using alcohol and tobacco also play a role in the development of foot ulcers.
Ulcers form due to a combination of factors, such as lack of feeling in the foot, poor circulation, foot deformities, irritation (such as friction or pressure), and trauma, as well as duration of diabetes. Patients who have diabetes for many years can develop neuropathy, a reduced or complete lack of ability to feel pain in the feet due to nerve damage caused by elevated blood glucose levels over time. The nerve damage often can occur without pain, and one may not even be aware of the problem. Your podiatrist can test feet for neuropathy with a simple, painless tool called a monofilament.

Vascular disease can complicate a foot ulcer, reducing the body’s ability to heal and increasing the risk for an infection. Elevations in blood glucose can reduce the body’s ability to fight off a potential infection and also slow healing.
Symptoms
Because many people who develop foot ulcers have lost the ability to feel pain, pain is not a common symptom. Many times, the first thing you may notice is some drainage on your socks. Redness and swelling may also be associated with the ulceration and, if it has progressed significantly, odor may be present.
Dr. Corey LeJeune discusses Diabetic Foot Care. The doctors at OCFA are top rated. The Podiatry Center is top rated in Orange County, CA.
When to Visit a Podiatrist
Once an ulcer is noticed, seek podiatric medical care immediately. Foot ulcers in patients with diabetes should be treated to reduce the risk of infection and amputation, improve function and quality of life, and reduce health-care costs.

Diagnosis and Treatment
The primary goal in the treatment of foot ulcers is to obtain healing as soon as possible. The faster the healing, the less chance for an infection.
There are several key factors in the appropriate treatment of a diabetic foot ulcer:
- Prevention of infection
- Taking the pressure off the area, called “off-loading”
- Removing dead skin and tissue, called “debridement”
- Applying medication or dressings to the ulcer
- Managing blood glucose and other health problems
Not all ulcers are infected; however, if your podiatrist diagnoses an infection, a treatment program of antibiotics, wound care, and possibly hospitalization will be necessary.
To keep an ulcer from becoming infected, it is important to:
- Keep blood glucose levels under tight control;
- Keep the ulcer clean and bandaged;
- Cleanse the wound daily, using a wound dressing or bandage; and
- Avoid walking barefoot.

Dr. Daphne Yen treats a Podiatry patient in Orange County.
For optimum healing, ulcers, especially those on the bottom of the foot, must be “off-loaded.” You may be asked to wear special footgear, or a brace, specialized castings, or use a wheelchair or crutches. These devices will reduce the pressure and irritation to the area with the ulcer and help to speed the healing process.
The science of wound care has advanced significantly over the past ten years. The old thought of “let the air get at it” is now known to be harmful to healing. We know that wounds and ulcers heal faster, with a lower risk of infection, if they are kept covered and moist. The use of full-strength betadine, hydrogen peroxide, whirlpools, and soaking are not recommended, as these practices could lead to further complications.
Appropriate wound management includes the use of dressings and topically-applied medications. Products range from normal saline to growth factors, ulcer dressings, and skin substitutes that have been shown to be highly effective in healing foot ulcers.
For a wound to heal, there must be adequate circulation to the ulcerated area. Your podiatrist can determine circulation levels with noninvasive tests.

Tightly controlling blood glucose is of the utmost importance during the treatment of a diabetic foot ulcer. Working closely with a medical doctor or endocrinologist to control blood glucose will enhance healing and reduce the risk of complications.
Surgical Options: A majority of non-infected foot ulcers are treated without surgery; however, if this treatment method fails, surgical management may be appropriate. Examples of surgical care to remove pressure on the affected area include shaving or excision of bone(s) and the correction of various deformities, such as hammertoes, bunions, or bony “bumps.”
Healing time depends on a variety of factors, such as wound size and location, pressure on the wound from walking or standing, swelling, circulation, blood glucose levels, wound care, and what is being applied to the wound. Healing may occur within weeks or require several months.

Prevention
The best way to treat a diabetic foot ulcer is to prevent its development in the first place. Recommended guidelines include seeing a podiatrist on a regular basis. Your podiatrist can determine if you are at high risk for developing a foot ulcer and implement strategies for prevention.
You are at high risk if you have or do the following:
- Neuropathy
- Poor circulation
- A foot deformity (e.g., bunion, hammer toe)
- Wear inappropriate shoes
- Uncontrolled blood sugar
- History of a previous foot ulceration

Reducing additional risk factors, such as smoking, drinking alcohol, high cholesterol, and elevated blood glucose, are important in prevention and treatment of a diabetic foot ulcer. Wearing the appropriate shoes and socks will go a long way in reducing risks. Your podiatrist can provide guidance in selecting the proper shoes.
Learning how to check your feet is crucial so that you can find a potential problem as early as possible. Inspect your feet every day—especially the sole and between the toes—for cuts, bruises, cracks, blisters, redness, ulcers, and any sign of abnormality. Each time you visit a health-care provider, remove your shoes and socks so your feet can be examined. Any problems that are discovered should be reported to your podiatrist as soon as possible; no matter how simple they may seem to you.
The key to successful wound healing is regular podiatric medical care to ensure the following “gold standard” of care:
- Lowering blood sugar
- Appropriate debridement of wounds
- Treating any infection
- Reducing friction and pressure
- Restoring adequate blood flow
Diabetic Foot Care Guidelines
Diabetes can be dangerous to your feet – even a small cut can produce serious consequences. Diabetes may cause nerve damage that takes away the feeling in your feet. Diabetes may also reduce blood flow to the feet, making it harder to heal an injury or resist infection. Because of these problems, you may not notice a foreign object in your shoe. As a result you could develop a blister or a sore. This could lead to an infection or a non-healing wound that could put you at risk for an amputation.
RELATED PAGE: Diabetic Shoes and Orthotics
To avoid serious foot problems that could result in losing a toe, foot, or leg, follow these guidelines:
- Inspect your feet daily. Check for cuts, blisters, redness, swelling, or nail problems. Use a magnifying hand mirror to look at the bottom of your feet. Call your doctor if you notice anything.
- Wash your feet in lukewarm (not hot!) water. Keep your feet clean by washing them daily. Use only lukewarm water – the temperature you would use on a newborn baby.
- Be gentle when bathing your feet. Wash them using a soft washcloth or sponge. Dry by blotting or patting, and carefully dry between the toes.
- Moisturize your feet – but not between your toes. Use a moisturizer daily to keep dry skin from itching or cracking. But DON’T moisturize between the toes – that could encourage a fungal infection.
- Cut nails carefully. Cut them straight across and file the edges. Don’t cut nails too short, as this could lead to ingrown toe nails. If you have concerns about your nails, consult your doctor.
- Never treat corns or calluses yourself. No “bathroom surgery” or medicated pads. Visit your doctor for appropriate treatment.
- Wear clean, dry socks. Change them daily.
- Avoid the wrong type of socks. Avoid tight elastic bands (they reduce circulation). Don’t wear thick or bulky socks (they can fit poorly and irritate the skin).
- Wear socks to bed. If your feet get cold at night, wear socks. NEVER use a heating pad or hot water bottle.
- Shake out your shoes and feel the inside before wearing. Remember, your feet may not be able to feel a pebble or other foreign object, so always inspect your shoes before putting them on.
- Keep your feet warm and dry. Don’t let your feet get wet in snow or rain. Wear warm socks and shoes in winter.
- Never walk barefoot. Not even at home! Always wear shoes or slippers. You could step on something and get a scratch or cut.
- Take care of your diabetes. Keep your blood sugar levels under control.
- Don’t smoke. Smoking restricts blood flow in your feet.
- Get periodic foot exams. Seeing your foot and ankle surgeon on a regular basis can help prevent the foot complications of diabetes.